The method of diagnosis and correction - which later became known as orthomanual medicine - turned out to be successful.
In 1971 I had worked out the consequences of pelvic obliquity. This occurs after strain involving unilateral prolapse of the sacrurn relative to the osilium. To cope with this oblique basis, the spinal column rotates around the longitudinal axis, alternately towards the right and the left, up to and including C-5. This was published in the "Nederlandsch Tijdschrift van Geneeskunde" ("Dutch Journal of Medicine").
The inadequacy of roentgen diagnostics in this case is striking. In the ‘70s it was quite normal to find serious postural abnormalities upon orthomanual examination in young people with multiple complaints, but with very normal X-rays, who had consequently been referred to a psychiatrist. Since the sympathetic nerve passes directly along the spinal column and a blocked vertebra is surrounded by a substantial amount of oedema (as far as the point of the spinous process!) it is not surprising to find a connection between organ dysfunctions and vertebral displacements in the segments belonging to the organs. An article on this was published in the Dutch journal "Integrale Geneeskunde" ("Integral Medicine"). The sacral parasympathetic plexus also plays a role. Stimulation of this, by abnormalities in the pelvis after a fall and/or serious displacements of L-5 to L-4, causes unwanted weight increase; published in "Arts en Alternatief" ("The Physician and Alternative Medicine").
Lastly, in the early '90s I came across a not so very common serious displacement of C-1 relative to C-2 in my patients. These patients had back complaints elsewhere in the spinal column and were also depressed. I was intrigued and now systematically examined each patient for this abnormality and found it more often. When asked, "Do you also feel depressed?" they consistently responded in the affirmative. Some of them had inexplicable fits of weeping, some had panic disorders, anxieties and nightmares, while others suffered from depressed mood and diminished activity, but they all had complaints of this nature in varying intensity.
Background
In the '50s, the possibility of vertebral blocks was pointed out to me by a
physiotherapist who practised manual therapy. It seemed a logical idea to me, given the many unergonomic forces imposed on the spinal column in some sports and accidents.
I referred patients to him and placed myself under his treatment when I incurred intercostal neuralgia in the seventh month of pregnancy. In the ensuing years I noticed improvements in the patients treated by him but no striking changes in posture. When, seven years later, I again became pregnant and (this time in the fifth month) came down with the same intercostal neuralgia, in 1965 I decided to make a closer study of this subject.
I proceeded on the basis of anatomic principles, since the correct anatomy of the joint results in the correct function. I could also - once I had established the deviation from the normal position - rectify the abnormality with light pressure in exactly the right direction, determined by the abnormal position that had to be corrected.
I subsequently found that many other systems of manipulation are based on the functional limitations of the joint as a diagnostic guideline.
Reasons for the research
In my research, which was published in the journal "Integrale Geneeskunde", apart from gastrointestinal complaints, heart function disorders and lung conditions, I also included hyperventilation and migraine. In migraine a statistically significant connection was found between this illness and displacements of C-7 and T-1. This concerned stimulation of the ganglion cervicale inferior (stellatum). If both vertebrae were straight, no migraine occurred. Upon relapse of the displacement (e.g. through overload of the right arm) the migraine returned (and consequently so did the patient for repeat treatment). Furthermore, not everyone with migraine responds to this displacement, not by any means. There is probably a hereditary factor present here.
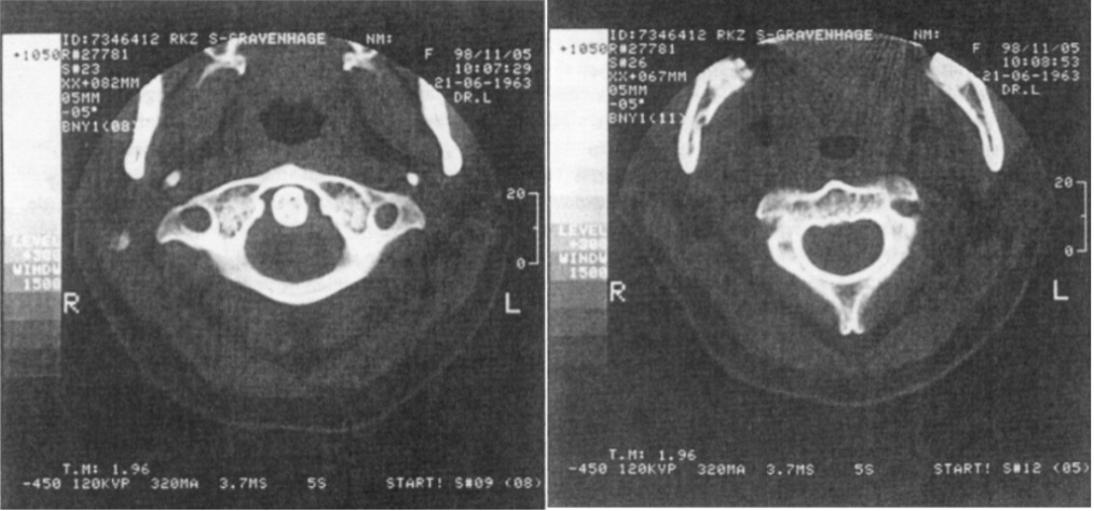
Subsequent examination revealed that this is not so surprising, because the abnormality discovered concerns a unilateral to ventral dislocation of C-1 on C-2 (see photos), causing substantial stretching of the ligamenturn transversurn atlantis. However... ahead of both transverse processes of C-1 and C-2 the ganglion cervicale superior is situated, which is vigorously stimulated by this position! The nervus vagus also exits the cranium through the foramen jugulare, which is situated just ahead (ventrally) of the transverse processes of C-1. With a normal position of C-1 the nervus vagus passes straight along the transverse processes of C-1 to the caudal extremity. In the displacement of C-1 discussed here, the nervus vagus is depressed ventrally and therefore chronically mechanically stimulated.
I had relieved a kitchen installer of his back complaints and depression (when there is a brief history of depression it responds rapidly to correction of the displacement). This man returned again complaining of depression after he had struck the back of his head forcibly against an overhead kitchen cabinet during installation work and, indeed, the displacement was back again! Together with the fact that I had meanwhile seen and treated about 150 patients with this abnormality plus depressive disorders, this
decided me to contact the Brain Institute in Amsterdam. At this point I would especially like to thank my colleague J. v.d. Ende for acting as intermediary.
Research
Prof. R. Buys of this institute showed an interest and he proposed that I should conduct a trial with the Beck's Depression Inventory (BDI test). This is a generally accepted questionnaire containing 21 questions. Prof. Buys advised: "Let the patients complete the questionnaire and repeat this several weeks later to see whether the depression is extremely variable. Then you treat some of these patients immediately and some of them later for the C-1 abnormality, thus enabling any difference between these two groups to be established. Follow-up these patients for a few years by means of the BDI questionnaire, then we can see the result".
The 21 questions dealt with the following subjects: sadness, future perspective, sense of self-esteem, pleasure in life, guilt feeling, feeling of being punished, suicidal tendency, tendency to weep, feeling for irritation, interest in others, decisiveness, self-image, energy, sleeping disorders, fatigue, appetite, weight loss, healthcare and interest in sex. The questions were ranked in four degrees, increasing from slight to severe. For each question one could therefore score from 0 to 3 points.
To my surprise I saw that there were no questions about anxiety and no questions
about nightmares. I added these questions with the same ranking as in the BDI. The course of the use of antidepressants was also noted.
Most of the patients also had an abnormality which occurs after a whiplash injury. I will publish a study on this at a later date. Three patients moreover had a serious abnormality of the head-atlas position, combined with the homolateral whiplash abnormality. I call this combination the Fatal Combination and a more detailed study on this will likewise be published at a future date.
The patients involved in the trial can be typified as follows:
Group 1 consisted of ten women between 34 and 62 years of age (mean age 45.5) and seven men between 48 and 64 years old (mean age 52). Of these women, two had incurred their depression following childbirth (postnatal depression). They both stated that during childbirth considerable pressure had been exerted on the back of the head in order to press down harder, while the chin was already in contact with the chest. In this way, of course, the abnormality is easily produced: during parturition all ligaments have maximum elasticity! Of this group of men and women, 12 patients were taking antidepressants.
When the first group clearly responded to correction of the displacements, after a few months a SECOND GROUP was started, consisting of 19 women between 23 and 68 years of age (mean age 42) and four men between 36 and 54 years old (mean age 43). This group therefore comprised a total of 23 subjects. Of this second group, one female patient had the fatal combination and seven women were suffering from PND, with the same story about the cause of the abnormality as the women in the first group. Of this second group, 15 patients were taking antidepressants. The entire trial therefore comprised 40 patients, of whom nine women with PND and 27 patients taking antidepressants. Of these 40 patients, 27 also had a whiplash abnormality (WL). Of the nine PND patients, three also had a whiplash abnormality.
Most of the patients were ready with spine-correction after three treatments (needless to say, the whole of the spine was corrected). Upon registration the patients were sent a BDI questionnaire. They received their first treatment a few weeks later. A BDI questionnaire was completed on this occasion too. I only gave the first two treatments in quick succession, after which I treated C-1 in 20 patients during the first session and not in the other 20 patients. Between the second and third treatment there was an interval of four weeks. At the third treatment session the patients again completed a BDI questionnaire and the twenty not C-1 treated patients got there C-1 correction. so four and a half week later than the other twentypatients. The patients subsequently completed a questionnaire every three months for a few years. The first questionnaire completed at home and the questionnaire completed during the first visit were averaged and these figures were taken as the initial reference data. Incidentally, relatively few differences were found between the two questionnaires; in other words, the depressions were fairly stable. The first figure is the BDI figure. The + symbol is followed by the figure for my two anxiety questions.
Since a study conducted by the Brain Institute (4) had shown that changes occur in the brain tissue in endogenous depression, one may assume that the changes will increase the longer the depression lasts when the underlying cause is indeed a persistent anatomical deviation. Owing to the displacement of C-1, the ligamenturn transversurn atlantis is stretched; in other words, due to pressure on the occiput, for example by turning over in bed the wrong way (supporting the body on the head and heels), or because of pressure in the neck from the edge of the washbasin at the hairdresser, C-1 can again became displaced.
Results
Initially, the C-1 of half of the patients was treated straightaway; the other patients were later treated. The mean BDI starting score of the treated group was 22, while the untreated group scored 23. Both groups were therefore quite comparable.
| C1 threated | score start |
score after 1 month |
score after 3 months |
score after 22 months |
| yes 20 subjects | ||||
| no 20 subjects |
The improvement of 6 points in the treated group was clearly significant (p value < 0.005). The untreated group showed a decrease of 3 points. This figure is still significant (0.025< p<0.05).
From this we see that the non-treated group also responded. Most of these patients were in the group that was first treated. Since in many cases the social situation of these subjects was also jeopardised by the depression, there was considerable relief that something at least was happening. The placebo effect in medication is estimated at 30%. But that is by no means the case here. After three months the treated group dropped from 16 to 14, while the non-treated group shows a catching-up effect from 20 to 15 (p<0.005). This effect is continuing: after nearly two years a further improvement has occurred.
The following table shows the results of the patients, classified in groups according to the duration of their illness. The table indicates the number of patients per group, the mean BDI score plus the number of patients taking antidepressants (M) at the start of the trial and at the end of the trial, as well as the improvement, expressed as a percentage, in both the BDI questions and the anxiety questions.
| Duration of depression |
Number of patients |
Starting score | Number M | End score | Number M | Improvement |
| >30 years | 29 + 3,6 | 6 patients | 16 + 2,0 | 2 patients | 36% + 44% | |
| 20-30 years | 17 + 2,5 | 3 patients | 10 + 1,5 | 1 patients | 43% + 40% | |
| 10-20 years | 23 + 3,4 | 5 patients | 8 + 1,6 | 3 patients | 66% + 53% | |
| 5-10 years | 22 + 2,8 | 7 patients | 7 + 1,2 | 3 patients | 66% + 57% | |
| <5 years | 17 + 2,75 | 6 patients | 6 + 1,4 | 4 patients | 62% + 49% |
Discussion
This table shows that the longer the illness lasts the higher the BDI score and the lower the improvement percentage. This also applies to the anxiety questions. In particular, there is a marked difference in recovery when the disorder has been in existence for more than 20 years. However, consideration should be given to the fact that these patients are as a rule also older, as a result of which the recovery can be slower.
All patients in the trial responded favourably. This is an important difference with treatment with medication, which shows 33% to be non-responders (5). It should also be noted that the trial started and ended in the winter.
The stretched ligamenturn transversurn atlantis does mean that the patient must be wary of exerting pressure on the occiput, in order to avoid a relapse. Relapses occurred regularly in half of the patients during the years that the trial was conducted, mostly in chronic depressed subjects. They then experienced pressure in the occiput and a rapid return of the feelings of depression. After coming back for treatment, they quickly recovered.
| Duration of illness |
Number of patients |
Mean BDI with C1 displaced |
3 weeks after recovery C1 |
| >30 years | |||
| 20-30 years | |||
| 10-20 years | |||
| 5-10 years | |||
| <5 years |
As this table shows, all groups clearly responded to the treatment; however, in this short term (3 weeks) the anxieties clearly do not respond as well as the depressive symptoms, i.e. the parasympathetic hypertonia goes away faster than the sympathetic hypertonia.
The abnormality can be seen on the images of the scans shown here. When making the scan, care should be taken to ensure that the patient keeps his head straight, i.e. in line with the L axis. Because of the abnormality he will feel that his head is turned to one side. The patient's head should therefore be fixed while the images are made.
Conclusions
With this trial I believe I have demonstrated that there is a clear connection between the reported abnormal positions of C-1 and vital depression. An average improvement of 55.9%, while half of the patients (on their own initiative) no longer use, antidepressants, is a fairly good result, the more so since 32 of the 40 patients may be placed in the category of protracted chronic patients. Of great importance is the fact that the mechanical stimulation of the ganglion cervicale superior offers a perfect explanation for the increase in the cortisol producing cells in the PVN region of the brain found at the Brain Institute (4). Further to this publication, the cortisol content in the blood was determined in 19 patients prior to treatment. A higher level was only found in one patient who had been ill for less than five years.
It is also to be expected that parts of the tractus parasympathicus in the brain stem will display increased activity, as explained in the foregoing. The inactivity of the depression points to increased parasympathetic activity, while anxiety is more a sympathetic stimulus phenomenon.
I would like to thank my colleague J. v.d. Ende for his constructive criticism and Dr. C.W. Aakster for checking the statistical data.
Literature
- Sickesz and Bongartz, Orthomanuele Geneeskunde, Nederlandsch Tijdschrift van Geneeskunde, 133, p. 928.
- M. Sickesz, Correlatie tussen orgaanfunctiestoornissen en wervelfoutstanden, een prospectief onderzoek. Tijdschrift voor Integrale Geneeskunde, 1994, p. 195.
- M. Sickesz, Relatie tussen lichaamsgewicht en sacrale dysbalans, een prospectief onderzoek. Arts en Alternatief, 1993, no. i-2, p. 22.
- Purba J.S., Hoogendijk W.J.C., Hofma M.A. and Swaab D.F., Increased number of vasopressin neurons in the paraventricular nucleus of the human hypothalamus in depression. Archives of General Psychiatry, 1996, 53, p. 137-143.
- De Jonghe and Swinkels, Antidepressiva, 1995, p. 116, ISBN 90-73637-25-2.