The uncomplicated whiplash abnormality comprises points 2 and 3. The orthomanual practitioner manipulates these abnormalities and corrects them in three sessions.
The enclosed scans show abnormalities 2 and 3. When making the scans, care should be taken to ensure that the head is positioned absolutely straight. Due to the abnormality the patient tends to turn his head because, for him, he feels that this is the "straight" position.
General
The cause of a whiplash injury does not necessarily have to be a car crash. Any accident in which the head snaps backwards can result in the following abnormalities. The whiplash abnormality usually occurs on the left side and will accordingly be described as such in this article (see points 2 and 3).
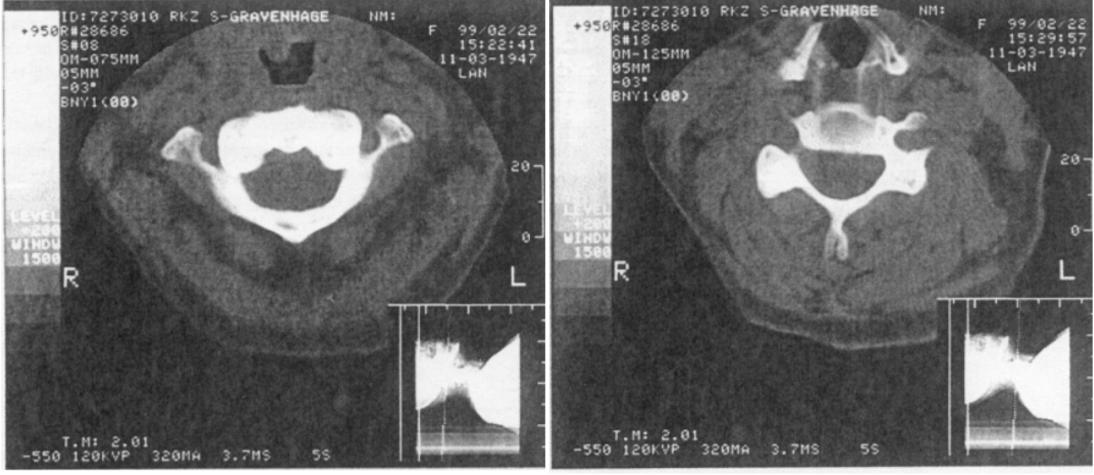
One should also realise that in this examination the patient is lying down, while the abnormality I have described is in a patient in the seated position. The asymmetric pressure of the head, which weighs several kilos, is therefore eliminated in the former position and this is why the abnormality cannot be seen on an X-ray image until a later stage.
Research
Three months after treatment, forty patients with a whiplash injury were asked about the results. Of these patients, 26 had the uncomplicated abnormality, 6 had the complication as described under 1) and 10 had the complication as described under 4). From this it may be concluded that 2 patients had both complications. The patients were subsequently asked whether they had experienced any of the following ten complaints:
- Cranial neuralgia: headache on top of the head; the dermatome of C-2 is the scalp.
- Occipital neuralgia: the dermatome of C-3 is the neck and the occiput.
- Dizziness: via irritation of the ganglion cervicale superior, which is situated against the transverse processes of C-1 and C-2 on the ventral side, vascular spasms can occur in the brainstern and these can also cause the complaints as described under 3, 4, 5, 9 and 10.
- Concentration disorders.
- Sleeping disorders.
- Impaired mobility of the neck.
- Snoring: the front end of the vertebrae forms the back of the throat. Since vertebral misalignments cause oedema around the vertebra which is visible at the dorsal side up to the point of the processus spinosus, the back of the throat will therefore also be oedematous: an oedema which may even extend as far as the uvula. This may explain complaints 7 and 8.
- Sleep apnoea.
- Facial neuralgia.
- Tinnitus.
The examined group of subjects consisted of 28 women and 12 men.
Their age distribution was as follows:
10-20 years, 2 patients; 20-30 years, 6 patients; 30-40 years, 9 patients; 40-50 years, 7 patients; 50-60 years, 11 patients; 60-70 years, 2 patients; 70-80 years, 3 patients.
The duration of the complaints was as follows:
Less than 5 years, 22 patients; 5-10 years, 8 patients; 10-20
years, 6 patients; 20-30 years, 4 patients.
Discussion
When the abnormality has already existed for more than 10 years, a check-up after three months is of course fairly quick. Especially in elderly patients, one can imagine that recuperation of the ligament and muscle apparatus and the resorption of oedema can take slightly longer.
With regard to points 3, 4 and 5, other causes may have a hand in the matter; this also applies to points 7 and 8 (e.g. allergy), point 9 (inflammation of the jaw) and point 10 (inner ear problems). Nonetheless, it turns out that whiplash injury also scores high in these complaints as the causative agent.
The question now, of course, is what an orthomanual treatment can do for patients who have had complaints for more than 20 years and for the elderly. Here are the results:
- Man, born on 4/8/71. 20 years' complaints as described under 1,2 en 3. Now free of complaints.
- Woman, born on 11/7/60. 20 years' complaints as described under 2, 3, 4, 5, 6, 7, 8, 9 and 10. Complaints as described under 3, 4, 7 and 10 now improved; the rest have been eliminated.
- Woman, born on 22/6/43. 23 years' complaints as described under 2, 3, 4, 5, 6, 7 and 8. Complaints as described under 4 and 7 now improved; the rest have been eliminated.
- Woman, born on 17/12/26. 20 years' complaints as described under 1, 2, 3 and 6. Complaints as described under 2 and 6 now improved. Complaints as described under 3 unchanged; the complaint as described under I has been eliminated.
- Woman, born on 14/3/26. 10 years' complaints as described under 1, 2, 4, 6, 7 and 8. Now free of complaints.
- Woman born on 18?/3/25. 4 years' complaints as described underl, 2, 3, 5, 7, 9 and 10. Now a significant improvement in complaints as described under 2 and 10; complaint as described under 5 unchanged; the rest have been eliminated.
Of the patients who had both complications the results are as follows:
- Man, born on 27/3/47. 8 years' complaints as described under 1, 2, 3, 4, 5, 6, 7, 8 and 10. Complaints as described under 3, 4, 5 and 10 unchanged; complaint as described under 6 improved; the rest have been eliminated.
- Man, born on 23/1/67. 12 years' complaints as described under 3, 4, 5, 6 and 10. Complaint as described under 4 now improved; complaint as described under 5 unchanged; the rest have been eliminated.
| Number | Eliminated | Improved | Unchanged | |
| 1) CRANIAL NEURALGIA | ||||
| 2) OCCIPITAL NEURALGIA | ||||
| 3) DIZZINESS | ||||
| 4) CONCENTR. DISORDERS | ||||
| 5) SLEEPING DISORDERS | ||||
| 6) MOBILITY | ||||
| 7) SNORING | ||||
| 8) SLEEP APNOEA | ||||
| 9) FACIAL NEURALGIA | ||||
| 10) TINNITUS |
In conclusion, for interested colleagues a description is given below of the precise manoeuvres needed to correct this abnormality The sequence of the manoeuvres must be followed exactly. The following applies to a left-sided abnormality.
Session 1
C-2 is completely fixed on C-3 (no translation), whereby the left caudal facet joint fixes in the left cranial facet joint of C-3; the vertebra rotates around the AP axis towards the left and in the L(ong) axis towards the right. We call this the L(uxated) D(orso) P(osition).
- Patient in the right lateral decubitus position with the head supported by a pillow. Stand behind the patient and using your right thumb press the processus spinosus of C-2 downwards. This disengages C-2 from C-3.
- Position the patient on his left side and repeat this manoeuvre with your left thumb. This neutralises the left rotation in the AP axis. C-4 is in a R(otated) D(orso) P(osition), which means that the right caudal facet of C-4 engages the right cranial facet joint of C-5. To neutralise this:
- Patient in the ventral decubitus position with the chin pointing towards the chest and the head in the head supports of the couch. Stand at the end where the patient's head is situated, place your left thumb under the right processus transversus of C-4 (i.e. against the ventral side) and press it in the dorsal direction; then, using your right thumb, press the left processus transversus of C-4 towards the median line.
Session 2
- Repeat manoeuvre C of the first session, only this time with C-2 because the LDP of C-2 has changed to an RDP. So you do not get C-2 in the correct position straightaway.
- Position the patient on his right side without a pillow and with the head hanging down over the shoulder. Stand behind the patient and using your left thumb press the left processus transversus of C-3 in the ventral direction. This is necessary in order to neutralise the right rotation around the L axis. In its LDP, C-2 has also taken C-3 and C-4 with it in a right rotation. We call this the S(coliosis) P(osition).
Session 3
Repeat the manoeuvres in session 2, only this time with C-3 in A) and C-4 in B).
And with this the uncomplicated whiplash abnormality has disappeared. In essence, this abnormality is a half scoliosis unit of C-2: in a scoliosis situated lower in the spinal column the two vertebrae above the LDP are also included in the abnormality.
When the complications as described under 1 and under 4 have occurred, you proceed as follows:
For an abnormality as described under 1): at the end of the session 1 you continue with manoeuvre D) with the patient in the dorsal decubitus position. Have an assistant apply light traction to the patient's head and press with a thumb the processus transversus of C-1 in the dorsal direction at the side where C-1 is (most) ventrally positioned. If necessary, repeat this on the other side in session 2. The processus transversus of C-1 is situated one centimetre in the cranial direction from the angulus mandibulae, just under the point of the petrosal bone.
For an abnormality as described under 4): at the end of the session 2 you continue with manoeuvre C) with the patient in the dorsal decubitus position. Stand behind the patient and using your right thumb press the right processus transversus of C-2 in the dorsal direction. This is situated at the level of the angulus mandibulae With this misalignment you can feel the processus rising in the ventral direction relative to the processus transversus of C-3. Position the patient on his left side and press the processus spinosus of C-2 to the left.
At the end of session 3 you continue with manoeuvre C: with the patient in the ventral decubitus position and traction applied by an assistant, press the left processus transversus of C-2 in the ventral direction.
Lastly, I must seriously warn against the tendency of ordinary manual therapists to press the transverse process of C-2 (the painful protuberance for the patient) in the ventral direction. All that one achieves by this is to push the atlas at that side under the cranium, with the Fatal Combination as a result! (See the following article.)